Thalamotemporal Alteration and Postoperative Seizures in Temporal Lobe Epilepsy
Abstract
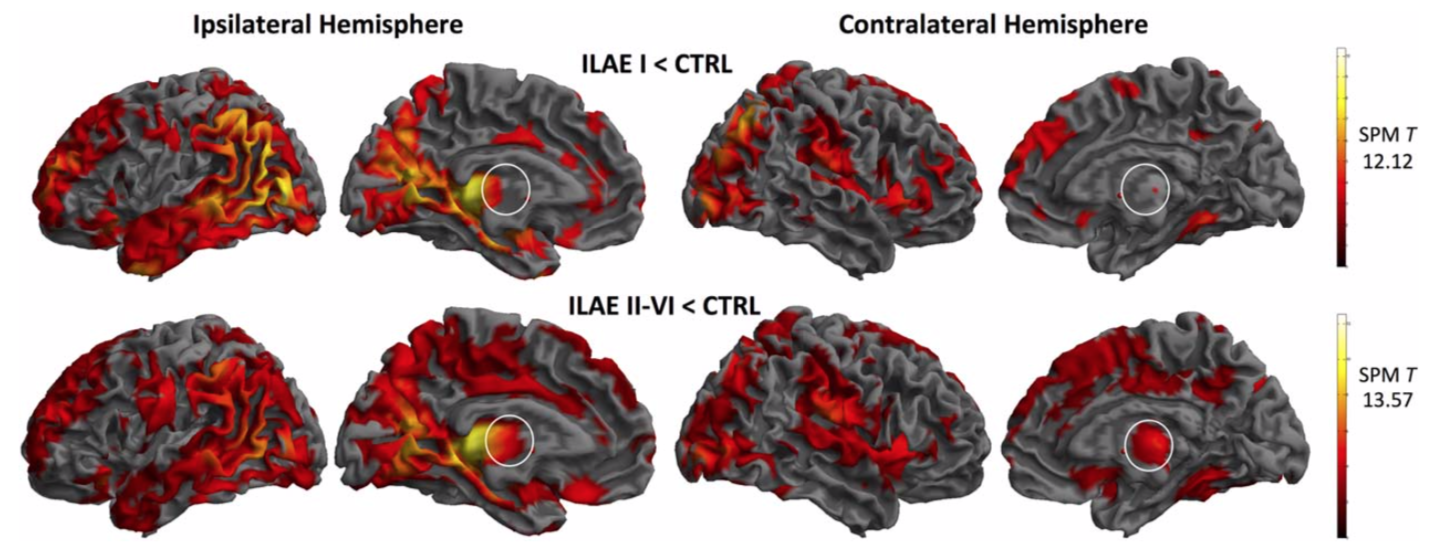
Objective: There are competing explanations for persistent postoperative seizures after temporal lobe surgery. One is that 1 or more particular subtypes of mesial temporal lobe epilepsy (mTLE) exist that are particularly resistant to surgery. We sought to identify a common brain structural and connectivity alteration in patients with persistent post-operative seizures using preoperative quantitative magnetic resonance imaging and diffusion tensor imaging (DTI). Methods: We performed a series of studies in 87 patients with mTLE (47 subsequently rendered seizure free, 40 who continued to experience postoperative seizures) and 80 healthy controls. We investigated the relationship between imaging variables and postoperative seizure outcome. All patients had unilateral temporal lobe seizure onset, had ipsilateral hippocampal sclerosis as the only brain lesion, and underwent amygdalohippocampectomy. Results: Quantitative imaging factors found not to be significantly associated with persistent seizures were volumes of ipsilateral and contralateral mesial temporal lobe structures, generalized brain atrophy, and extent of resection. There were nonsignificant trends for larger amygdala and entorhinal resections to be associated with improved outcome. However, patients with persistent seizures had significant atrophy of bilateral dorsomedial and pulvinar thalamic regions, and significant alterations of DTI-derived thalamotemporal probabilistic paths bilaterally relative to those patients rendered seizure free and controls, even when corrected for extent of mesial temporal lobe resection. Interpretation: Patients with bihemispheric alterations of thalamotemporal structural networks may represent a subtype of mTLE that is resistant to temporal lobe surgery. Increasingly sensitive multimodal imaging techniques should endeavor to transform these group-based findings to individualize prediction of patient outcomes.